As a medium, VR is still finding its legs across many industries including gaming, enterprise, and fitness. Meanwhile, researchers at the New York-based Icahn School of Medicine at Mount Sinai are beginning to link VR therapy to a growing bank of knowledge regarding gamified rehabilitation.
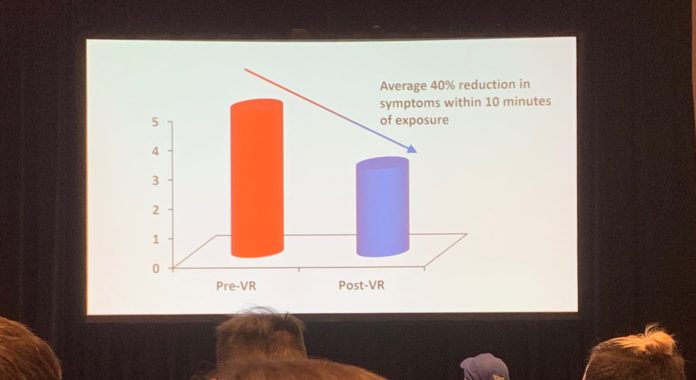
At last month’s Game Developers Conference (GDC), Neuroscience Ph.D David Putrino detailed significant findings that he and his team at Mount Sinai gathered while studying the effects of VR on pain patients. Basically, Putrino’s team discovered an average 40% rate of symptom reduction in pain patients across their tests, each administered for 10 minutes a piece.
In contrast, Putrino and his team claim that less than 30% of patients suffering from neuropathic pain experience relief from traditional medications (such as opiates).
The ultimate goal of the Mount Sinai research team is to develop ways to completely subvert a need for chemical substance-based treatments in chronic pain patients. As with a separate team of Providence researchers, and Dr. Brennan Spiegel of Cedars-Sinai, who each found similar results within VR. I promise to get into the meat of what’s going on in Putrino’s findings, but before I do, let’s first swing by one of his past TEDx Talks for some supporting context:
In this video, Putrino explains the underlying concept of neuroplasticity (inarguably crucial to understanding how VR therapy interacts with pain), admitting to his audience that he himself “was paralyzed on the entire left side of his body,” after he’d stopped breathing for multiple minutes at 18 months of age.
“Our brains are made out of brain cells; we call these neurons, and these neurons team up to produce many different functions,” Putrino explains in the opening moments of his speech. “So my work and the work of many other scientists have shown that you need a big team of neurons together to produce movement. Unfortunately, when you have brain damage, that team is broken.”
“Now, it’s not all bad news; the brain has the ability to recover,” Putrino continues. “What [neuroplasticity] means is that some neurons that survive the initial damage can form new teams. They can reach out to other neurons in the brain nearby that do similar things and pull them into a new team. And sometimes, if the brain gets it just right, that new team can be just as effective as the old team—sometimes even more effective.”
Walking this understanding of neuroplasticity back to Putrino’s talk at GDC, the team at Mount Sinai attributes their success to what are essentially just fun activities that can motivate patients to get their neurons firing together again, building new neural pathways that help them overcome pain. And, ultimately, without exposing those patients to costly or potentially addictive substances.
But how is VR therapy supposed to work in practice? Well, the concept of ‘mirror neurons’ can clue us in on what connects fun activities with the revitalization of neural connections in the brain.
To draw in even more supporting context, I found an interesting article in the International Archives of Medicine, published in 2013, which details the relationship between mirror neurons and stroke survivors in rehab. The researchers in that study concluded that “mirror neurons are involved in imitative learning through interactions with neural motor areas in humans.” Meaning that, as we understand them, mirror neurons allow humans to both mimic the behavior of other humans and learn from our environments through observation.

We can assume that mirror neurons look for stimuli to imitate and latch onto. Under that assumption, once that source is found, the mirror neurons jump into action and begin polarizing other neurons nearby. But as those researchers put it more specifically, “the mirror neuron system interacts with vision, proprioception and motor commands, promoting the recruitment of mirror neurons and the cortical reorganization and functional recovery of post-stroke patients.”
And that’s where VR comes in.
Essentially, when a pain patient experiences a total context switch—so that there’s something entertaining or relaxing to distract them while the environment (in this case, the VR app) coaxes them to engage the underlying cause of their pain—they’re getting a chance to exert agency as if they had complete, painless access to that part of their body.
During his GDC presentation, Putrino referred to the work of neuroscientist Vilayanur Ramachandran, who created the ‘mirror box‘ studies that showed positive findings in amputees who were given a mirrored illusion of their non-amputated limbs. Seeing their limbs reflected in the mirror supposedly allowed those amputees to relieve their chronic phantom limb pain, which gave Putrino plenty of data about the efficacy of using virtual avatars to achieve the same effect.
At this point, it’s safe to say that those mirror neurons aren’t simply a testament towards the human brain’s incredible ability to repair itself—they’re critically important for scientists like Putrino to promote while developing new pain treatments such as (but not limited to) VR therapy.
That said, he only holds that it’s important for the patient to be able to observe and (physically) interact with the therapeutic activity—not that they must necessarily be inside of VR to reap the benefits of mirror therapy. “I think we don’t even need to go as far as VR. We just need motion capture systems that give people continuous feedback about how they’re moving,” Putrino told the audience during his presentation at GDC, in reference to motion capture systems such as the Microsoft Kinect.
“One of our control conditions is actually viewing [these experiences] on a 2D screen, because if we can do this in 2D, let’s totally do this in 2D,” Putrino later told a member of the crowd while fielding questions.
But while Putrino believes that the results of his VR therapy study at Mount Sinai can be reproduced in 2D, others believe that there’s something uniquely ‘VR’ about his team’s results. Kevin Bruggeman, a Graduate Research Assistant at The Ohio State University College of Arts and Sciences (where he applies his background as a 3D graphics designer, in collaboration with a psychologist and a neuroscientist, to create immersive content for healthcare applications), has his own insights into what’s made VR therapy show positive results across the board thus far.
“It’s the minimization of distraction and the ability to engage on multiple levels [that’s specific to VR],” Bruggeman told me while we both sat down for lunch together at GDC. “When you’re in VR, you’re dealing with a higher sensory level. If you’re watching a [2D] screen and there’s a relaxing environment on the screen, you can look left and right and you’re no longer in an immersive space. You don’t feel a sense of presence in that space.”

“VR is very much in its infancy stage, and yeah there are issues, but realistically what needs to happen for inpatient care is mobile VR,” Bruggeman continued. “Doctors can’t do the base stations for every hospital room and go through all the setup it requires—it’s just not feasible.”
And while VR has shown promise for treating chronic pain, Putrino presses importance on the fact that “there’s no silver bullet for any condition, least of all pain.” In the Mount Sinai lab, researchers work with many high-performance athletes, an example that he’s happy to use while extrapolating his findings with general pain patients. “When I have a well-championed athlete that doesn’t want to do a certain exercise, I find a different exercise for them,” Putrino said to a GDC audience member just moments before his allotted speaking time ran out. “If they’re not feeling it from the first session, I gotta do something else with them because I know right there and then that it’s not gonna work.”

“I was having a conversation with a VC the other day about another pain intervention that we’re running through clinical trials in my lab,” Putrino continued. “And the VC said ‘I only want to invest if it’s definitely going to work on at least 80% of pain patients,’ and I said ‘Well then don’t invest in anything in pain because that’s just not a reasonable thing to experience,’ and we hold the same in all aspects of rehabilitation.”
Whether it be robotic rehabilitation, gamified rehabilitation, or just regular old conventional OTPT, Putrino puts high importance on the fact that while some people respond to a particular treatment, other people don’t. “Some people have preferences—go with their preferences.”
There are still certain kinds of pain, such as chronic neuropathic pain, which need more research before they can be treated. That’s an example of a specific type of pain that’s present with about 80% of chronic spinal cord injury patients, Putrino says, and neither opiates nor virtual reality have shown any positive results towards treatment. And while he and his team are working on some possible treatments for those patients, they involve experimental technologies that are unrelated to virtual reality.
While VR Fitness Insider rarely covers pain as a core subject, it’s still a critical part of understanding the connection between the human body and VR, especially when it comes to telegraphing, managing, and resolving the injuries associated with chronic physical stress (caused inside or outside of virtual reality). Back in October, we covered a similar study conducted by The University of Kent, which resulted in a positive outlook for VR as a pain reduction tool. Furthermore, if you’re interested in reading more about this subject, I recommend taking a look into our coverage of the Neon VR and AR apps, which are designed specifically to tackle chronic pain.
Have you or anybody you know successfully used VR to relieve chronic pain? Let us know in the comments.